The Erosion of Clinical Practice in the NHS: How Protocols and Untrained Staff Allegedly is deemed as "Quakers"
- Author
- Kadiyali Srivatsa
- Published
- Fri 06 Jun 2025
- Episode Link
- https://rss.com/podcasts/srivatsa/2061472
The Erosion of Clinical Practice: How Protocols and Untrained Staff Allegedly Undermined Medical Training in the NHS
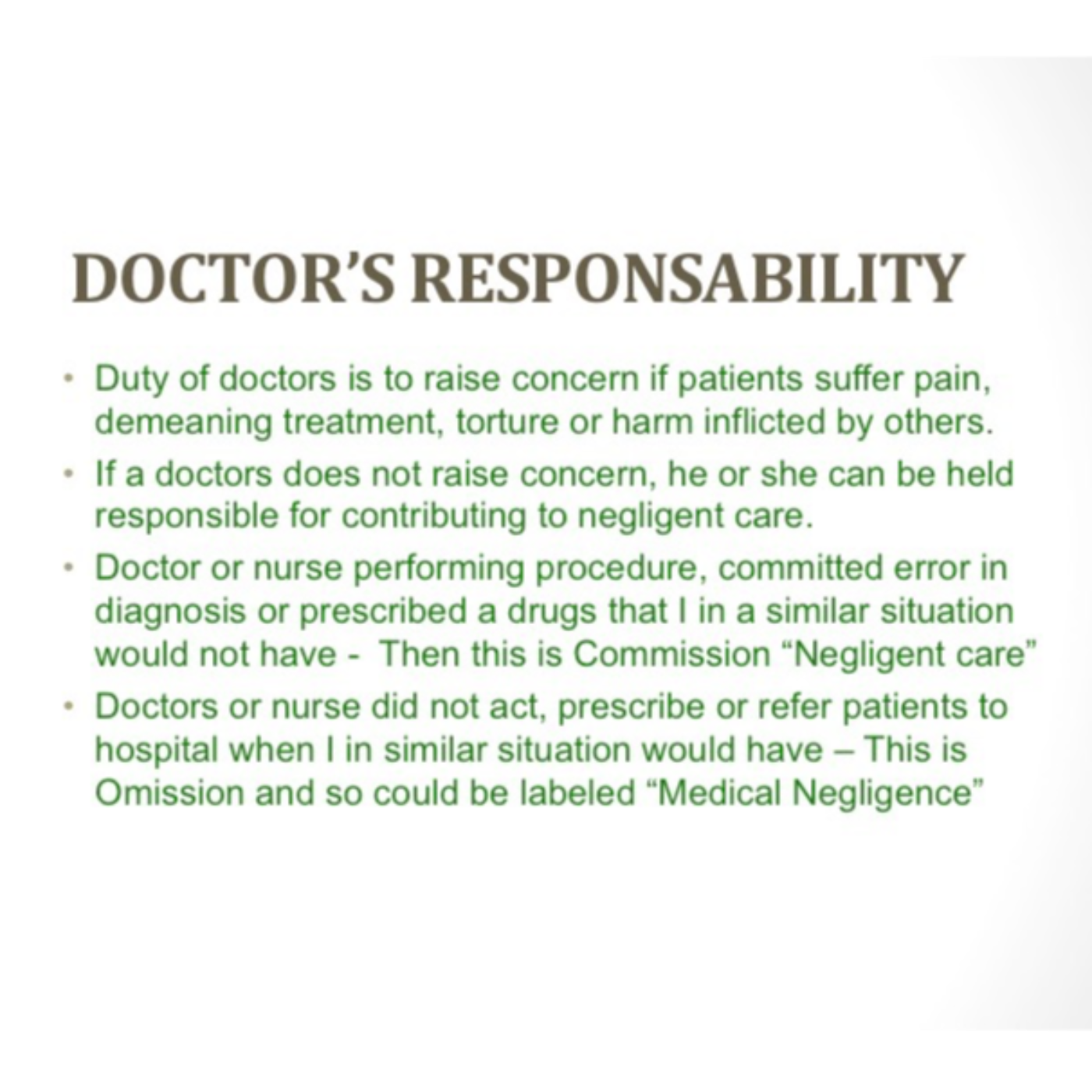
For decades, the UK's National Health Service (NHS) has been celebrated for providing free healthcare at the point of need. However, according to one doctor's perspective detailed in the sources, changes in recent years have allegedly led to a decline in the quality of care and ethical standards, particularly impacting medical training and patient safety. This narrative highlights a shift from traditional, human-centred clinical practice towards protocol-driven approaches and increased reliance on non-medically trained staff.
The Introduction of Preprinted Assessment Sheets. He wrote, "When patients describe the symptoms for which they seek professional attention, they are also reporting the story of an illness as they have lived and remember it, and so it can vary". He asserted that a doctor must listen to the story of illness and offer a solution, not a prescription.
He also reminded doctors that we must not forget that doctors trained today will be our doctors tomorrow, so they will be better doctors who can help us when we retire. Unfortunately, this has not occurred, but we are encountering sub-standard healthcare in the NHS.
The Influence of Evidence-Based Medicine and Protocols
The narrative suggests that this shift towards structured data collection coincided with or was influenced by the growing dominance of evidence-based medicine (EBM). EBM, which emphasizes the systematic analysis of published medical research as the basis for clinical decision-making, particularly bestowing "gold standard" status on randomized controlled trials (RCTs), has been widely incorporated into clinical practice, training programs, and policy development. While proponents describe EBM as integrating the best available evidence, clinical expertise, and patient values, criticisms mentioned in the sources include that EBM can sideline clinical expertise and patient values with protocolized, algorithm, and guideline-based treatments.
The Rise of Non-Medical Practitioners and Alleged Substandard Care
The situation was reportedly exacerbated by the introduction of nurse-led practices and the licensing of nurses and chemists to diagnose and prescribe drugs. Dr Srivatsa recounts being invited to work in a "Pilot Nurse-led Practice" in 2003 to train and certify nurses to diagnose infections and prescribe antibiotics, accepting in the hope of validating his innovation, "Maya". However, he felt uncomfortable because patients consulting nurses in these practices allegedly returned with complications.
The doctor's journey, marked by early formative experiences, a commitment to traditional clinical skills, raising concerns about perceived declining standards and patient safety, facing institutional opposition, and ultimately developing a technological solution, is presented as a fight for medical ethics, the doctor's oath, and the protection of humanity in the 21st century.
#DrMayaGPT #SelfDiagnosis #PreventiveCare #PatientEmpowerment #AIinHealthcare #WomensHealthAI #HealthEducation #FutureOfMedicine #DigitalHealth #HealthcareRevolution #PublicHealth #PandemicPreparedness #MedicalEthics #TearsOfHappiness #HealWithMaya #YourAIHealthCompanion #ListenToHeal #TrustYourSymptoms #NHS #GMC