📝 “How Do You Manage Chest Pain & Dyspnea Post-Op IV Sedation?”
- Author
- Brendan Gallagher, DDS
- Published
- Mon 25 Aug 2025
- Episode Link
- https://podcasters.spotify.com/pod/show/doctorgallagher/episodes/How-Do-You-Manage-Chest-Pain--Dyspnea-Post-Op-IV-Sedation-e379l5t
Quick Review #284 - #anesthesia #sedation #surgery #doctorgallagher #oralsurgery #oralsurgeon #omfs #dentist #dentistry
- 8.25.25
Post-operative chest pain and shortness of breath in a patient with hypertension undergoing IV sedation includes a differential diagnosis: myocardial infarction (MI), pulmonary embolism (PE), pneumothorax, and aspiration/airway compromise. Recognizing which diagnosis to rule out first is critical.
Step 1: Initial Assessment
Immediately stop all activity, reassess ABCs (airway, breathing, circulation), apply 100% oxygen, and place the patient on full monitoring (ECG, SpO₂, BP). Chest pain with dyspnea must be treated as a presumed cardiac event until proven otherwise.
Step 2: Prioritizing Differential
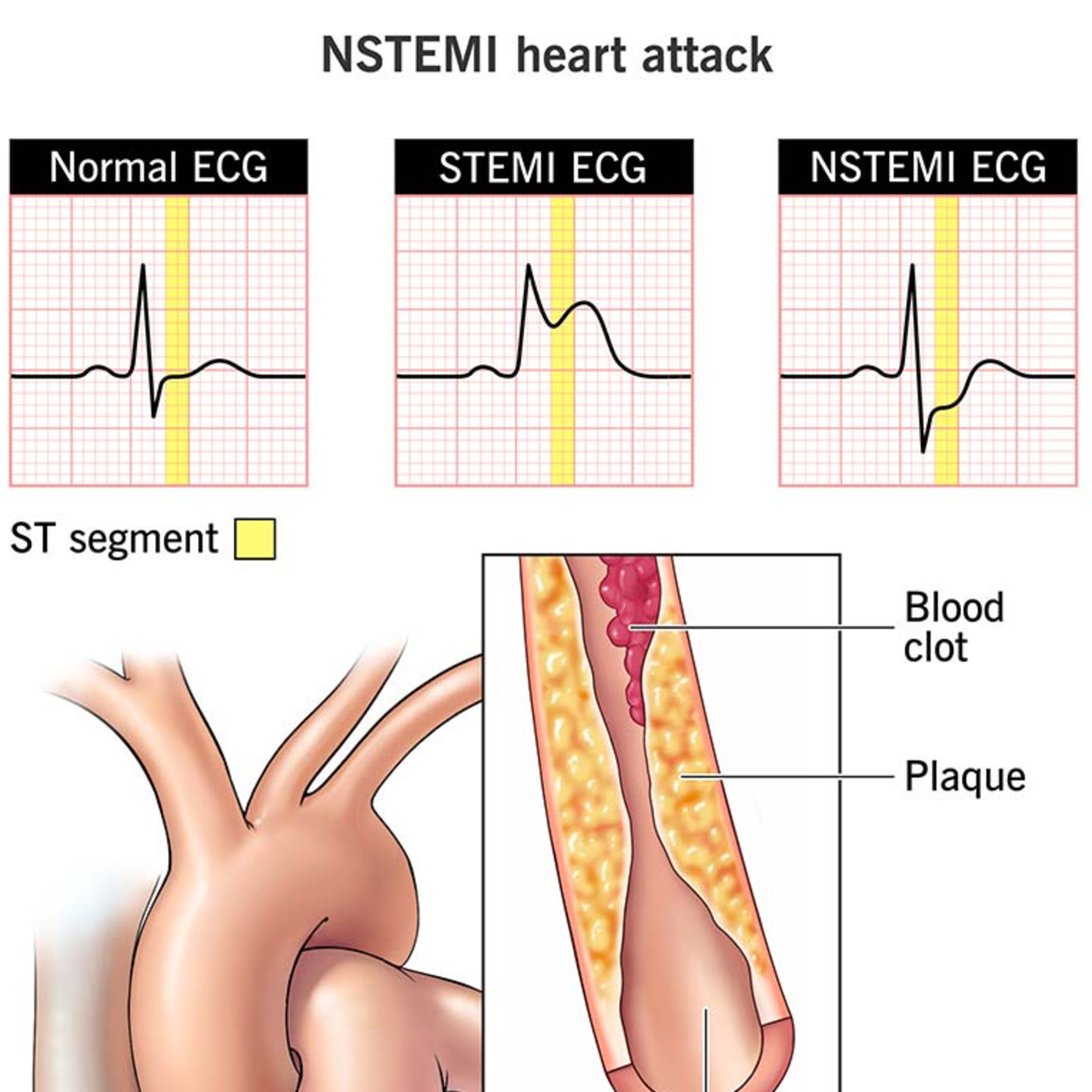
• MI/ACS is the most urgent to exclude. A hypertensive middle-aged male is high risk. Acute chest pain and dyspnea strongly suggest ischemia. Perform an ECG first, looking for ST elevations, T wave inversions, or new Q waves. Administer chewable aspirin (325 mg) if no bleeding risk, and consider sublingual nitroglycerin (0.4 mg) only if systolic BP >90 mmHg. Call EMS immediately — definitive management requires hospital transfer and possible reperfusion therapy.
• Pulmonary Embolism also presents with acute dyspnea and pleuritic chest pain, often post-op. Tachycardia, hypoxemia, and anxiety raise suspicion. However, diagnosis requires imaging (CT angiogram) not available in the office, making supportive O₂ and EMS transfer the main interventions.
• Pneumothorax can follow PPV or barotrauma. Signs include unilateral chest pain, absent breath sounds, and hypotension if tension physiology develops. Requires urgent O₂, EMS transfer, and if crashing, needle decompression.
• Aspiration/airway compromise is also possible, especially in sedation. Coughing, wheezing, or stridor point toward this. Immediate suctioning, airway maneuvers, and PPV with 100% O₂ are essential.
Step 3: Key Learning Point
The most immediate diagnosis to rule out is MI because it is both common and most rapidly fatal. The first test is ECG — fast, accessible, and diagnostic. PE, pneumothorax, and aspiration remain high-yield considerations, but they are second-line in acute triage.
References:
1. Cleveland Clinic. (2023). NSTEMI: Non-ST-elevation myocardial infarction (heart attack). Cleveland Clinic.
2. Miloro, M., Ghali, G. E., Larsen, P. E., & Waite, P. (2022). Peterson’s Principles of Oral and Maxillofacial Surgery (4th ed.). Springer.
3. Abubaker, A. O., Lam, D., & Benson, K. (2016). Oral and Maxillofacial Surgery Secrets (3rd ed.). Elsevier.
4. ChatGPT.2025.
#podcast #dentalpodcast #doctor #dentist #dentistry #oralsurgery #dental #dentalschool #dentalstudent #dentistlife #oralsurgeon #doctorgallagher