📝 “How Do You Manage Bradycardia With Hypotension in IV Sedation?”
- Author
- Brendan Gallagher, DDS
- Published
- Sat 23 Aug 2025
- Episode Link
- https://podcasters.spotify.com/pod/show/doctorgallagher/episodes/How-Do-You-Manage-Bradycardia-With-Hypotension-in-IV-Sedation-e377c5s
Quick Review #183 - #anesthesia #surgery #surgeon #doctorgallagher #oralsurgery #oralsurgeon #omfs #bradycardia
- 8.23.25
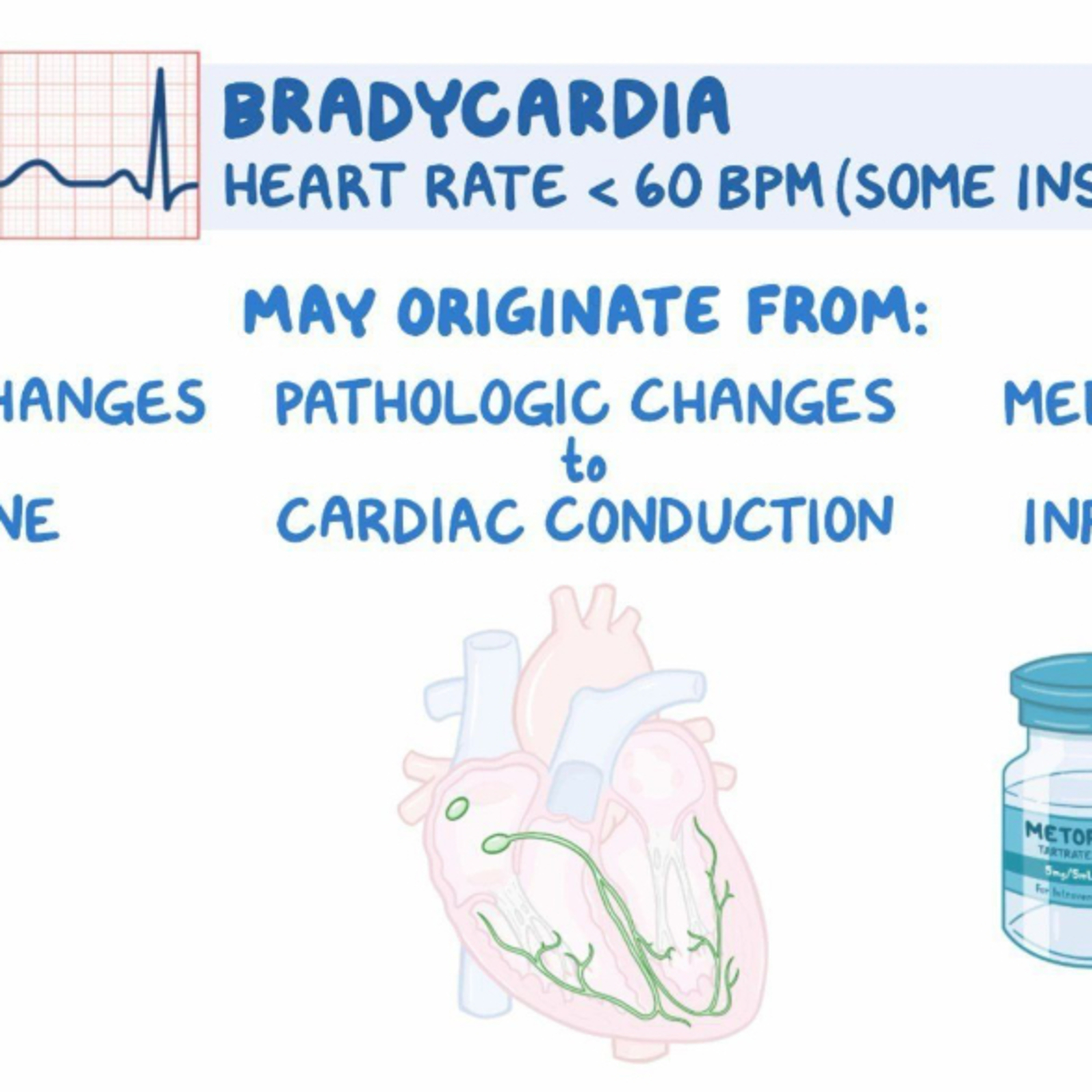
Management of bradycardia with hypotension during IV sedation requires rapid recognition and a stepwise approach because seconds can determine whether the patient stabilizes or deteriorates. The scenario involves a patient who becomes pale, with BP 90/50 and HR 40, while under sedation. This combination reflects inadequate cardiac output and oxygen delivery.
#1 - First step is airway and oxygenation. Immediately stop sedation drugs such as propofol or fentanyl that may be depressing respiration or cardiac function. Apply 100% oxygen via non-rebreather mask, and confirm airway patency. Hypoventilation and hypoxia can drive bradycardia and hypotension, so airway support comes before pharmacology. Monitoring SpO₂ and ETCO₂ is critical to identify hypoventilation early.
#2 - Second, circulation support. Establish IV access and give a rapid fluid bolus (e.g., 500 mL normal saline) if no contraindication like heart failure. This supports preload and perfusion while addressing possible vasodilation or intravascular depletion.
#3 - Third, pharmacologic intervention. For HR 40 with symptomatic hypotension, the drug of choice is Atropine 0.5 mg IV push, repeatable every 3–5 minutes to a maximum of 3 mg. Atropine blocks vagal influence on the SA node, increasing HR and improving cardiac output. Importantly, phenylephrine is avoided because, as a pure α-agonist, it can increase afterload but worsen reflex bradycardia. Epinephrine is reserved for cardiac arrest or refractory anaphylaxis, not first-line for isolated bradycardia with a perfusing rhythm.
#4 - Fourth, reassess and escalate. If the patient fails to respond, prepare for advanced measures: epinephrine infusion, transcutaneous pacing, or EMS activation for hospital transfer. Always check ECG for underlying rhythm changes, but only after stabilizing airway, breathing, and circulation.
Key Takeaway: Sequence matters—airway and oxygen first, fluids for support, then atropine to directly treat bradycardia. Recognizing oversedation and preventing recurrence with careful titration and continuous monitoring are equally essential.
References:
1. Osmosis. (n.d.). Approach to bradycardia: Clinical sciences. Elsevier. Retrieved August 23, 2025, from https://lnkd.in/enGbptP9
2. Miloro, M., Ghali, G. E., Larsen, P. E., & Waite, P. (2022). Peterson’s Principles of Oral and Maxillofacial Surgery (4th ed.). Springer.
3. Abubaker, A. O., Lam, D., & Benson, K. (2016). Oral and Maxillofacial Surgery Secrets (3rd ed.). Elsevier.
4. ChatGPT.2025
#podcast #dentalpodcast #doctor #dentist #dentistry #oralsurgery #dental #dentalschool #dentalstudent #dentistlife #oralsurgeon #doctorgallagher