Rethinking Polycystic Ovary Syndrome. PCOS. Is PCOS an Epiphenomenon
- Author
- Pandiyan Natarajan
- Published
- Fri 05 Sep 2025
- Episode Link
- https://rss.com/podcasts/diabesity-decodified-is-food-the-root-cause-of-type-2-diabetes-mellitus-pandemic/2200798
PCOS is an Epiphenomenon
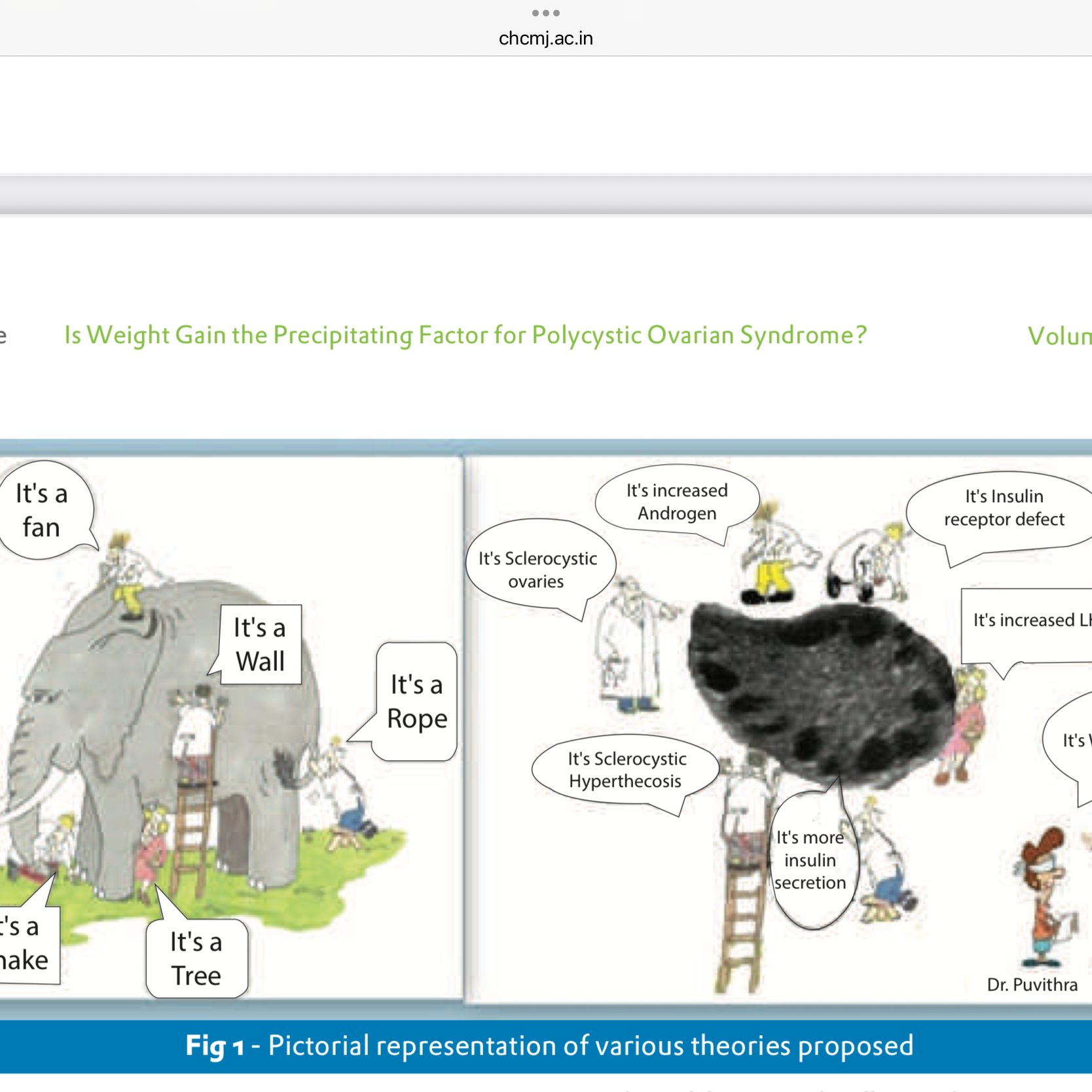
Polycystic Ovary Syndrome (PCOS), the commonest endocrine disorder in women, affects fertility, metabolism, & quality of life. It is portrayed as a primary disease of the ovaries, where follicles do not mature, ovulation becomes irregular, & multiple cysts appear on ultrasound. Is this the full story?
Our research over the past decade challenges this traditional view. We asked a simple question: Is PCOS the problem, or is it a downstream effect — an epiphenomenon — of something deeper?
Weight Gain Comes First
In our retrospective study of over 170 women with infertility, we noticed that more than 97% of women with PCOS had gained at least 4-5% of their body weight after adolescence before developing PCOS symptoms.
This weight gain was not limited to women who were overweight or obese. Even women with normal BMI developed PCOS when their weight crept up. Absolute number on the scale mattered less than shift in weight.
Why is this important? This suggests that weight gain may be the precipitating factor for PCOS. The ovaries, are not inherently diseased. Rather, they are responding to metabolic signals from rest of the body.
The Domino Effect: From Weight to Hormones to Ovaries
Biology supports this. Here is what happens when weight gain accumulates:
• More fat tissue increases leptin, which alters hypothalamic-pituitary-ovarian (HPO) axis.
• Rising blood sugar triggers insulin release & compensatory hyperinsulinemia.
• High insulin lowers sex hormone–binding globulin (SHBG), increasing the amount of free testosterone.
• Elevated free testosterone disrupts follicle development, leading to anovulation.
A Protective Checkpoint?
In a Perspective, we proposed that PCOS might serve as a biological checkpoint. By halting ovulation in a hormonally hostile environment, body may be protecting itself from high-risk pregnancies.
This reframes PCOS not just as a disorder, but as an adaptive response gone awry in the modern context of rapid weight gain & lifestyle change.
Pregnancy Complications: Blaming PCOS or BMI?
It is believed that women with PCOS are at higher risk for complications during pregnancy. Our 2017 study examined over 100 PCOS pregnancies compared to controls. The results were revealing:
• The only significant complication was gestational diabetes mellitus (GDM).
• Risk of GDM rose not because of PCOS itself, but in proportion to BMI.
• PCOS women with normal BMI had similar outcomes to non-PCOS controls.
Conclusion: PCOS is not an independent culprit. It is weight gain & metabolic status that drive both PCOS & its associated pregnancy risks.
Rethinking PCOS Management
If PCOS is an epiphenomenon of weight gain & metabolic dysfunction, then treatment strategies should shift focus:
• Instead of forcing ovulation through medications, we should address the root causes — weight management, insulin sensitivity,& lifestyle modification.
• By correcting upstream imbalance, downstream reproductive effects may resolve naturally..
Take-Home Message
PCOS may not be a disease of the ovaries. It may be the body’s way of signaling that something is off balance — a metabolic alarm bell ringing through the reproductive system.
When we ask, “Is PCOS an Epiphenomenon?” the evidence increasingly points to Yes. The shift in perspective could change the way we diagnose, counsel, & treat millions of women worldwide
- Disclaimer: This opinion article is for educational purposes only & does not constitute medical advice. Readers should consult their healthcare providers before making any decisions about diagnosis or treatment.